Coronary Artery Stenting
It is my view that world wide we do more coronary artery stent procedures than are indicated. Quite often a coronary artery stent will be deployed because there is a narrowing found in the coronary artery. However, the main use of coronary stenting is to improve symptoms such as angina, breathlessness, or documented lack of blood flow through that artery. In the absence of one of these features, there is no proven benefit to coronary artery stenting.
Why is Coronary Stenting performed?
Coronary artery stenting has become a very successful method for opening up coronary arteries that are limiting blood flow down the artery. Hence, patients who have symptoms such as angina or in the setting of a blocked artery leading to a heart attack, or if reduced blood flow down the artery is causing the heart not to function correctly, it is now possible in many situations to open the culprit narrowing using a standard coronary angioplasty and deploying a coronary stent to keep the artery open. There is very little justification in performing coronary stenting in patients who do not have any symptoms from the narrowed artery. Your doctor will assess whether the narrowed segment is suitable and whether performing a coronary artery angioplasty and stent is indicated in your particular case.
How is a Coronary Artery Stent performed?
Coronary Artery Stenting is performed in conjunction with a Coronary Artery Angiogram and hence the preparation and technique of this is similar, and is described in the section on Coronary Angiograms. After the preparation and the cannula is introduced into the groin (or arm), a special guiding catheter is advanced from the groin (or arm) and placed at the mouth of the coronary artery. A very fine guide wire is advanced down the coronary artery and over this an angioplasty balloon is advanced down the artery to the narrowed segment of the artery. Once appropriate positioning is established, the balloon is inflated with the stent over the balloon such that the stent is deployed into the wall of the artery. The balloon is then deflated and removed form the coronary artery. The stent will remain expanded forming an internal ‘scaffolding’ holding the artery open. Subsequent pictures are taken of the coronary artery to establish that an adequate result has been obtained. During inflation of the balloon and stent it is usual to experience some chest pain, possibly similar to the symptoms from before.
Depending on the complexity of the stent and the number of stents deployed, a stenting procedure may take 15 minutes to several hours longer than a standard diagnostic coronary angiogram.
What can I expect after coronary stenting?
Depending on the indication for Coronary Artery Stenting, you can expect rapid resolution of symptoms. You would be advised about the type and extent of activity you can perform immediately after a stent. It is usually advised that you can resume ordinary, everyday activities immediately, but should abstain from strenuous activity for a few weeks and often your doctor will recommend having a treadmill stress test 4-6 weeks after the stent to assess your exercise capacity.
It is IMPERATIVE that the medications you are commenced on at the time of your coronary stent, particularly aspirin and Plavix/Iscover be continued indefinitely and never to be ceased unless directed to by your Cardiologist.
What is Coronary Artery Stenting?
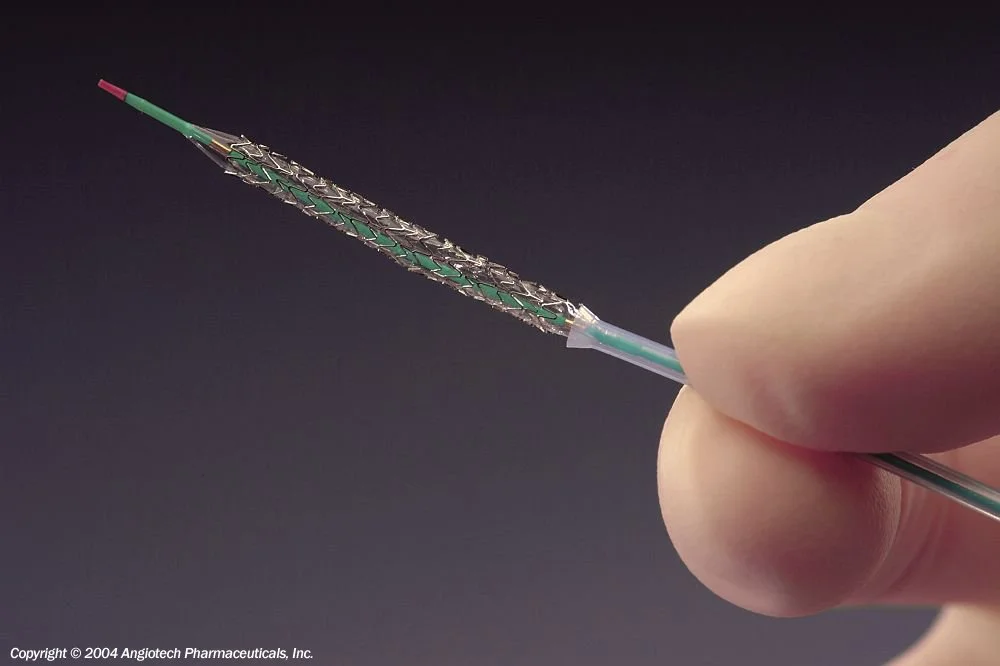
Coronary artery stenting is a technique to open up narrowed coronary arteries and to try and help them stay open. It is a technique that is performed in conjunction with Coronary Artery Angioplasty. A Coronary Angioplasty involves opening up a narrowed segment of a coronary artery using a small (2-4mm) elongated sausage shaped balloon within the narrowed segment such that is squeezes and forces open the coronary artery in that segment. However, because the coronary arteries have some degree of elasticity, often whilst the initial results look good, there was a significant incidence of recurrence of the narrowing in that area. In view of this, research led to the development of a coronary stents which are like a coil which when forced open gives the artery some structural support reducing the incidence of re-narrowing in that area.
Is there any preparation for a Coronary artery Stent?
Your doctor will discuss procedure with you prior to admitting you to hospital. You will be required to fast from midnight the night before the procedure. You should tell your doctor whether you have any allergies, particularly to iodide based substances. Your doctor will have discussed with you your medications, including diabetic medications such as insulin. He will give you appropriate instructions about these types of medications but most medications should be continued and brought to the hospital with you on the day of the procedure. You should be taking both Aspirin and a drug called Clopidogrel ( Plavix or Iscover) leading up to your Stenting.
What types of Stents are available?
Coronary Artery Stenting has become a highly successful technique with exceptionally good results. There are now two types of stent, commonly called either bare metal stents (BMS) or drug eluting stents (DES). The short term and long term results do differ depending on the stent used and in particular, differ depending on the type of artery, type of narrowing, size of artery and some other clinical features. Overall, for a bare metal stent there is an incidence of recurrent narrowing through the stent of approximately 10-30% which normally occurs within the first six months after the stent has been implanted. After this, it is very unusual for any further problems to occur in that area. In view of this, drug eluting stents (DES) have been developed. These are similar in structure to Bare Metal Stents but are coated with a drug than stops tissue growing through the stent causing further narrowing of the artery. This has reduced the chance of recurrence in the stented area in the first six months to as low as 1-3%. However, there is a small incidence of clotting within the stent after 1-2 years if certain medications are stopped. It is therefore a decision for you to take with your doctor, depending on the type of artery involved and your individual circumstances, about whether to elect for a bare metal stent or a drug eluting stent, although these days the majority of stents used would be the drug eluting stents.